Peace of mind
-
- from Shaastra :: vol 04 issue 01 :: Feb 2025

Understanding of schizophrenia has improved vastly in the past decade. New research and novel methods offer hope.
Ganesh Rajan was 19 when he developed auditory hallucinations. He remembers the early years — he calls them hell — when he couldn’t communicate with anybody. He has been on medication for 45 years since then, and has, over time, brought his condition under control.
Ganesh is a person with lived experience of schizophrenia. Today, he is a mental health volunteer with the Eklavya Foundation for Mental Health, Pune, and with SCARF India, the Chennai-based NGO.
Rajan’s suffering has made him more conscious of the need to speak up, especially in India, where mental illness is steeped in stigma. “If I can help a person in a similar situation to come out of this anguish, it would be a service I would pat myself for,” says the author of God Flipped Me Off: Schizophrenia Chronicle: A Story.
Medically, there are few interventions available for treating schizophrenia. However, the understanding of the condition has vastly improved in the past decade, triggering hope. In October 2024, the U.S. Food and Drug Administration (FDA) approved a new drug for schizophrenia.
Medically, there are few interventions available for treating schizophrenia. In October 2024, the U.S. FDA approved a new drug.
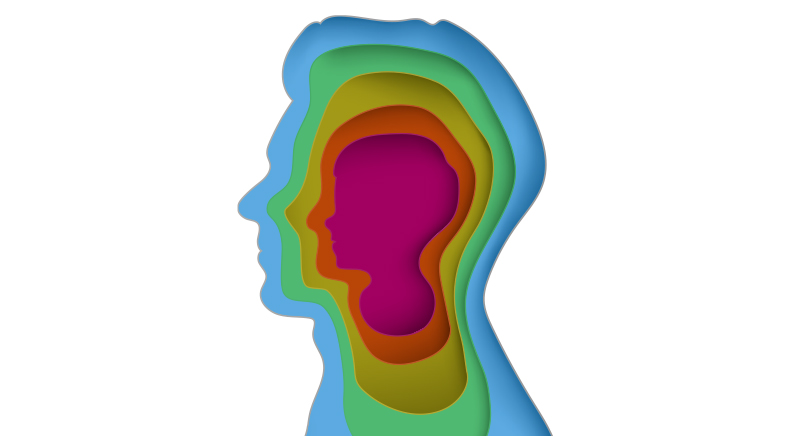
Schizophrenia is now seen as a complex and polygenic disorder. This means the symptoms are multi-pronged, and hundreds of genes are implicated. Researchers know there are changes in specific regions of the brain that raise the risk of a person developing symptoms. Underlying these brain changes are genetic abnormalities, known as single nucleotide polymorphisms (SNPs) or modifications in isolated genes. Unlike in many other diseases, where the presence of SNPs means the person is certain to develop a particular disease, in the case of schizophrenia, the SNPs only increase the risk of developing the illness. Schizophrenia may be triggered by external factors such as early childhood trauma, substance abuse or extreme stress during adolescence.
During adolescence, there is an excessive development of synapses or nerve junctions in the brain. Having an excess of such junctions renders the brain inefficient. So, to counter that, the human body undergoes synaptic pruning, or reducing the number of synapses. Excessive pruning or reduction of synapses, however, may raise the risk for schizophrenia.
DIFFERENT SYMPTOMS
A World Health Organization (WHO) factsheet on schizophrenia says it affects about 0.32% of people in the world (bit.ly/WHO-Facts). Yet, it is not adequately addressed by medical systems. What makes the situation more complicated is that it varies from individual to individual.
“Is it schizophrenia or schizophrenias,” asks M. Suresh Kumar, a psychiatrist from Psymed, a mental health hospital in Chennai. “People have different symptoms and signs, all put together under the rubric of ‘schizophrenia’.” Suresh Kumar refers to the four branches of symptoms that may be seen in a person with schizophrenia — positive, negative, cognitive and emotional. The positive symptoms may include persistent hallucinations and delusions; apathy and demotivation mark the negative symptoms. Symptoms of cognitive impairment show up as difficulty in carrying out tasks, and emotional disturbances manifest themselves as sadness, depression, fear, or anxiety.
For effective treatment, the four dimensions have to be understood comprehensively. However, medical interventions have targeted only the so-called positive symptoms. “Even with over 60 years of the drug (chlorpromazine) being in use, we do not have disease-modifying treatment options,” Suresh Kumar says. While there is research on disease-modifying interventions, clinical procedures are not available today.
Even the drugs being used are not diverse in their targets. They mainly target the symptoms of delusions and hallucinations. Most drugs that were available until today targeted only the so-called dopaminergic pathways. Dopamine, the target chemical, is secreted in the body, and is one of four important neurotransmitters needed for optimal brain function.
For long, studies have shown that schizophrenia is associated with increased dopamine signalling. Drugs that tackle this and target dopamine, especially its D2 subtype, are called Dopamine D2 agonists or inhibitors. Doctors have only recently been looking at other neurotransmitters — glutamate, gamma-aminobutyric acid (GABA) and acetylcholine. “Efforts to modulate glutamate or GABA could not translate into successful clinical medication, whereas dopaminergic modulators could,” says Ganesan Venkatasubramanian, Professor of Psychiatry and Consultant Psychiatrist at the National Institute of Mental Health and Neuro Sciences (NIMHANS), Bengaluru.
NEW CHANNEL
The drug approved by the FDA in October 2024 acts through a new channel (bit.ly/nature-fda). Called Cobenfy, it targets acetylcholine, another neurotransmitter, and more specifically, the M1 and M4 subtypes of acetylcholine receptors. Cobenfy is a combination of two drugs, xanomeline and trospium. This combination ushers in a new pathway to treat schizophrenia after nearly 70 years of medication consisting only of dopamine D2 agonists. People who did not respond to drugs available earlier may react well to the new drug. However, it essentially acts on the symptoms, specifically the positive ones.
“Disease-modifying interventions will be easier if the disease-causing processes were simpler,” says Matcheri Keshavan, Stanley Cobb Professor and Head of the Department of Psychiatry at Harvard Medical School. “However, since we know certain causal risk factors contribute... prevention may be possible.”
Diagnosis of the disease today is predominantly by clinical interviews. Researchers are now looking at genetic and blood-based tests and brain scans.
New research seeks to get to the bottom of the problem. Keshavan points out recent research indicating that oxidative stress, the process of production of energy by the brain, may be involved in disease causation. This process could be abnormal in affected persons, leading to the accumulation of toxic chemicals, which in turn may contribute to the disease processes. So, some current research is aimed at treating patients with antioxidants to control the progress.
“There are ways of improving cognition by brain training,” he says. There are different circuits in the brain, each with a function, such as those involved in memory, problem-solving, and so on. Using the property of neuroplasticity (the capacity to reorganise brain connections), the brain may be rewired in the case of malfunctioning circuits. “By appropriate computer-based exercises and through group and individual therapy, you can increase the brain’s capacity to function better.”
MODULATING BRAIN FUNCTION
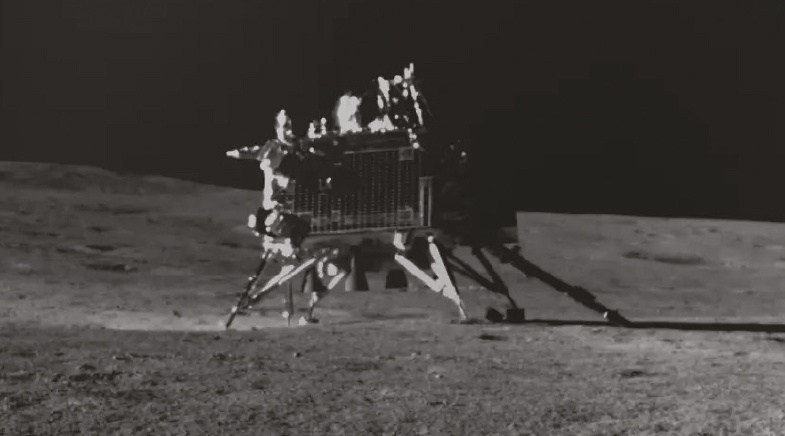
At NIMHANS, neuroscientists and psychiatrists are exploring the effect of what is called Transcranial Direct Current Stimulation (tDCS) to treat schizophrenia. This involves applying a weak direct current of about 2 milliamperes to specific areas of the brain to modulate brain function. This is done non-invasively using conductive silicone rubber electrodes over regions of the scalp which cover parts of the brain known to be abnormal in schizophrenia patients. “With this technique we have been able to treat medication-resistant auditory hallucination,” Venkatasubramanian says.
He explains that when treated with antipsychotic medication, nearly 70% of patients show noteworthy improvement. The NIMHANS researchers found that tDCS could reduce hallucinations in almost 50% of individuals who continue to have symptoms. “We are among the few centres in the world to utilise this technique to treat hallucinations in schizophrenia patients and report our results through systematic studies.” Now, the group is developing it into a clinical service.
Venkatasubramanian makes the critical distinction between tDCS and electroconvulsive therapy (ECT), commonly known as “shock treatment”. ECT uses a much higher current strength and requires anaesthesia, whereas in tDCS, the subject is conscious and cooperating throughout.
Diagnosis of the disease today is predominantly by clinical interviews. Researchers are looking at genetic and blood-based tests and brain scans. The brains of people with schizophrenia are examined using structural MRI methods, and these are compared with the brains of healthy subjects to find deficient volumes in multiple brain regions. Venkatasubramanian’s lab has also used the functional MRI method.
But these are group-level findings. “In a group of people, while a majority may have this problem, there are also people who show the profile we see in healthy subjects,” Venkatasubramanian explains. “We are yet to reach a stage when we can do a brain scan and say – ‘This is diagnostic of schizophrenia’.”
Meanwhile, there is a felt need for support systems. In 2024, Rajan participated in compiling the WHO’s Kathmandu charter on mental health (bit.ly/Kathmandu-charter). It focuses on how mental health patients ask to be treated, the rights of mental health patients, and what governments, bureaucracies, and employers can do to help. Altogether, it indicates the pathway towards better support systems for people with schizophrenia and greater acceptance of patients.
See also:
Have a
story idea?
Tell us.
Do you have a recent research paper or an idea for a science/technology-themed article that you'd like to tell us about?
GET IN TOUCH