Just breathe out
-
- from Shaastra :: vol 01 edition 03 :: Sep - Oct 2021

Medical advances have put the exhaled breath at the frontlines of efforts to diagnose killer diseases, and Indian scientists have joined the global quest.
A few years ago, a team of professors and research scholars at the Indian Institute of Technology Roorkee (IITR) deliberated over a few crucial questions. Could they create an affordable early warning sign for cancer? What if it alerted only users with a high probability of having cancer to seek medical advice before it was too late? What if it needed neither technicians nor machines?
There was clearly a felt need. Late detection compounds many common cancers. Consider lung cancer, globally the most commonly diagnosed type of cancer. A screening method for early detection, known as low-dose computed tomography (LDCT), needs expensive imaging equipment and trained staff to run it. In India, it usually costs at least ₹3,000 per test. In developing countries, issues of cost and access, and the danger of overdiagnosis, make mass screenings using LDCT a non-starter.
What if instead, the IITR team wondered, all that a screening test needed was a good long exhale?
Their queries - and the search for answers - led to the BLO detector, an unassuming, pocket-sized prototype that uses neither blood nor tissue but exhaled breath as a sample. A user blows into it and observes the resulting colour change in the material inside. This is matched to a colour sheet to detect the probability of three common cancers - breast, lung and oral. The device showed over 90% specificity and sensitivity in an initial study at a leading cancer hospital in Dehradun. The inventors envisage a cost of ₹100-200 per test though it is not yet final. "This should ideally be an over-the-counter test," says Siddharth Sharma, PhD scholar, Centre of Nanotechnology, IITR, and a co-inventor.
In New Delhi, Ranjan Nanda, Group Leader, Translational Health Group at the International Centre for Genetic Engineering and Biotechnology (ICGEB), has reached a turning point in a decade-long quest to identify a set of chemicals in the breath to detect tuberculosis (TB). He has finally identified 10 chemicals capable of discriminating between active TB and non-TB subjects (who may have some other respiratory disease) with roughly 90% accuracy. The ultimate goal, he says, is to put the science to work in a device that can even screen people at home.
WHIFF OF POSSIBILITIES
In the past decade or so, a growing number of researchers and companies globally have begun pushing hard to shape a future where exhaled breath leads to the early detection of diseases from infections to malignancies. It is a long haul, but their efforts are beginning to bear fruit, encouraging others. "The promise of being able to mine information from breath is massive," says Chandrasekhar Nair, Chief Technology Officer at the Goa-based Molbio Diagnostics, which has thrown its hat in the ring, too. "It can potentially help pick up disease early and fairly accurately, so it's exciting."
The COVID-19 pandemic has added another lens, through which breath-testing turns even more appealing. It is a rare opportunity for early movers to engage with regulators and quickly deploy breath tests. Companies working on breath analysis for cancer have smartly pivoted to COVID-19. A few tests have reached regulatory authorities for approval in Asia, Europe and the U.S.
"The lack of an easy, fast and affordable way to screen people at airports, arenas and social events has highlighted the need for rapid and real-time breath-based sensing," says Perena Gouma, Edward Orton, Jr., Chair in Ceramic Engineering at The Ohio State University (OSU), who has developed and published papers on breath sensors and devices over the past two decades. Her portable breath-testing device for COVID-19 is pending emergency approval in the U.S.
The BLO detector is an unassuming, pocket-sized prototype that uses neither blood nor tissue but exhaled breath as a sample.
Given the potential of breath analysis, "it's important to be in this field and have the capacity to do this," says Anurag Agrawal, director of the New Delhi-based Council of Scientific & Industrial Research-run Institute of Genomics and Integrative Biology (CSIR-IGIB). "It is now a question of effort and funding." CSIR-IGIB is a collaborator in a recent centre of excellence in breathomics funded by the Indian government at the All India Institute of Medical Sciences in New Delhi.
The world over, scientists and doctors are collaborating - collecting and sifting through breath sample data and published studies to understand the relationship between exhaled breath and diseases. In parallel, researchers and companies are trying a range of approaches to convert the science into actual breath tests. From using sophisticated analytical instruments to chemical nanosensors that mimic the human nose, disparate systems are being explored, and machine learning and artificial intelligence (AI) are being leveraged.
With huge advances in instrumentation, sensing and AI, it is now possible to imagine a future where the mysteries of breath are unravelled to positively impact disease and healthcare. "In the next few years, things are going to be good for the breath diagnostics development community," Nanda says. "There is a lot of activity, and I am quite hopeful."
Mass-produced, regulator-approved breath tests for a range of diseases are only five to six years away, says Hossam Haick, an expert in nanomaterial sensors and Full Professor in the Department of Chemical Engineering at the Technion - Israel Institute of Technology, Haifa. Breath analysis is now "mature" enough to begin that journey, says Haick, who has developed an AI-enabled electronic nose that is being tested in a range of diseases.
Significant challenges, of course, remain. But, first, why breath?
THE PROMISE
In the 1970s, Nobel Laureate in Chemistry Linus Pauling showed that human breath was a complex gas made up of hundreds of chemicals known as volatile organic compounds (VOCs). VOCs are the result of the body's biological processes, which can be altered by disease. Over the years, researchers have studied the presence and abundance of VOCs in exhaled breath as potential biomarkers - measurable indicators of disease. Some accepted ones are nitric oxide for asthma and carbon monoxide for neonatal jaundice. Exhaled breath also contains aerosolised droplets from the lungs' lining and particles that have non-volatile compounds such as proteins, which can also serve as biomarkers.
Breath analysis has several inherent advantages over other methods. One, it is non-invasive. This could improve patient compliance. "Obviously, it is easier to exhale than to suffer a pin-prick to provide a blood sample or having to provide a urine sample for testing," Gouma says.
Two, it has wide applicability. Breath-testing can be potentially used to detect a range of diseases from the infectious TB and COVID-19 to non-communicable ones such as cancers. Researchers have also analysed the breath of patients – with success – in an intensive care setting to detect ventilator-associated pneumonia and organ rejection.
Three, disease-linked changes in breath occur before symptoms appear, thus allowing early diagnosis. For instance, in studies, Haick's breath analyser could detect people with pre-cancerous lesions in gastric cancer.
Four, breath-testing lends itself to the creation of lab-independent, rapid tests. For instance, Singapore start-up Breathonix got a provisional regulatory nod in May to place its breath-testing equipment for COVID-19 at a checkpoint bordering Malaysia.
The world over, scientists and doctors are collecting and sifting through breath sample data and published studies to understand the relationship between exhaled breath and diseases.
Five, it can potentially aid precision medicine (see accompanying story: To the point). This is particularly useful for doctors treating complex diseases such as asthma where there are differences in how patient groups respond to the same therapy.
In the foreseeable future, established testing technologies will continue to provide the gold standard for diagnosis. The value of breath analysis will lie in addressing the unmet need to screen large volumes of people rapidly, using minimally trained or untrained hands, and at an affordable cost.
But if there is promise, there are impediments, too.
TREASURE HUNT
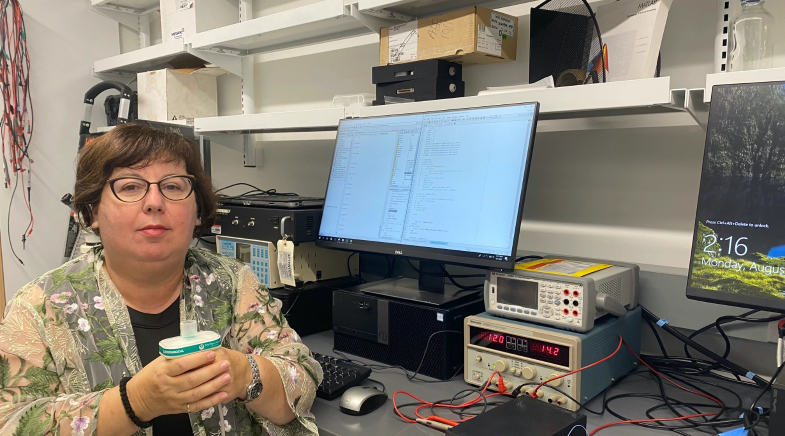
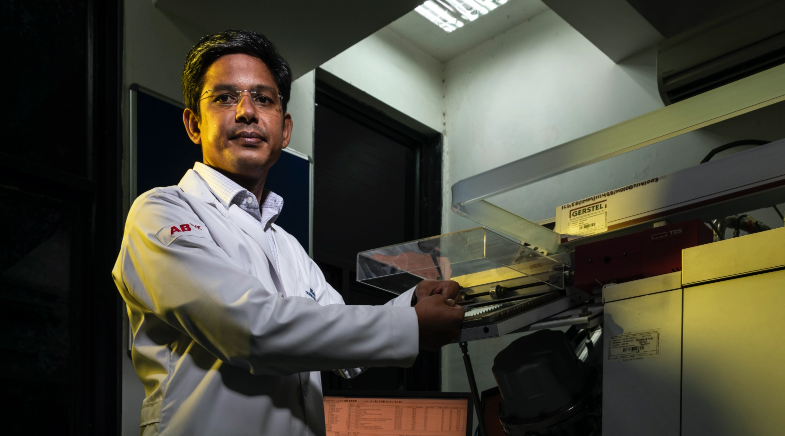
The first stumbling block is finding the right biomarkers. At ICGEB, Nanda's research has involved collecting exhaled breath samples of TB patients and controls (the healthy and those with other respiratory diseases) from different hospitals in the country in specialised steel tubes and running them through sophisticated Gas Chromatography-Mass Spectrometry (GC-MS) equipment in his New Delhi lab. Nanda says there are "critical challenges to capturing and analysing breath".
Human breath is a complex gas containing thousands of compounds in very minute quantities. These are known to be influenced by a range of factors such as diet and lifestyle. For instance, eating raw onions or drinking alcohol could lead to a higher concentration of sulphur and ethanol respectively in the breath. Pollutants in the environment, temperature and humidity also make a difference. Toluene in breath, for instance, may be from widely-used colour products such as paint or hair dye.
These variables confound researchers looking for true biomarkers. The "complexity and the large variations in people" mean that exhaled gas markers for most diseases remain "obscure", says Yangong Zheng, Associate Professor of Electrical Engineering and Computer Science Faculty in Ningbo University, China. His work with sensitive gas sensors and sensing algorithms that could potentially be used in an electronic nose for testing exhaled breath has made him an ‘impact creator' at the Institute of Electrical and Electronics Engineers, a global technical body (see box: Nosey marker).
There are ways to reduce some of these interferences. Subjects are asked to fast and stay away from alcohol or tobacco for a few hours before a sample is drawn. They may be asked to rinse their mouths with tap water. Taking a sample of the air in the room to establish a control data set also helps. Researchers use special bags or tubes to collect and transport samples. Nanda used tubes from European companies. During analysis, he discarded peaks on the MS graph formed by known environment contaminants, hospital indoor chemicals, plasticisers etc.
Nosey marker

Different gases are composed of molecules of diverse structures. In humans, these are matched to receptors in the nose that send a print to the brain, enabling it to identify a smell. However, unlike a dog's nose, which has many more receptors and, therefore, a wider olfactory range, the human nose has its limitations. E-noses were created to overcome these shortcomings of human olfaction using various types of nanomaterial-based sensors in a wide range of applications. Broadly, the sensors used could be acoustic, colorimetric or chemiresistors. These are capable of refined sensing in parts per billion, for instance. An e-nose typically has multiple sensors grouped in a specific way with the machine reading and recognising patterns. E-noses have been used to smell out explosives, detect poisonous gases in the air or toxins in sewer systems and even in judging the quality of tea. When it comes to breath analysis, the e-nose has some advantages over conventional lab testing instruments: it is portable and relatively cheap. However, e-noses for breath analysis are still being developed. Efforts are on to improve sensors and pair them with AI for better speed and accuracy of detection.
In some cases, researchers have combed through published studies to identify a single biomarker for a disease. For instance, the BLO detector contains chemicals that react with a single VOC in breath that is a product of malignant cells in specifically breast, lung and oral cancer, says co-inventor Indranil Lahiri, Associate Professor, Department of Metallurgical and Materials Engineering, IITR. Lahiri, who is on the faculty of IITR's Centre of Nanotechnology, did not name the VOC, citing confidentiality. He admits that there are "difficulties" in this approach as the published literature may often be contradictory.

A preferred approach is to look, like Nanda did, for breath prints or signatures. Nanda likens using a single marker to judging a student solely on math scores. A signature approach ensures that "if one marker underperforms, the others compensate for it." Nanda identified a panel of 10 biomarkers after collecting and analysing samples of patients with active TB, non-TB and healthy subjects from New Delhi, Manipur, West Bengal, Tamil Nadu and Tripura. He is preparing to publish his results.
With validated biomarkers or breath prints, the specificity of a test improves dramatically, Nair says. The higher the specificity, the lower is the rate of false positives. "You really don't want to alarm people (without cause)."
The difficulty in finding and validating biomarkers is one reason why there is still a large gap between the information available and actual tests, says T.S. Balganesh, a veteran Bengaluru-based scientist with experience driving innovation in government and industry labs. Geography and culture may be important factors in breath biomarkers, requiring longitudinal cohort studies in specific groups. "Given the diversity of populations, without Big Data analysis, we will be doing thousands of (biomarker) validations and shooting in the dark," he says.
MANY ROADS
Equally important is how the science will reach the patient.
It's open season right now. "Any technology that can selectively identify the metabolite of choice can be used," says Nair. "Till we do a lot more work on this we will not know what the best method is." As Gouma says, the creation of a new breath test calls for concerted effort by clinicians, scientists, sensor and devices experts, and breath analysis visionaries. "You have to identify and validate biomarkers, create selective sensors for them, validate the sensors with clinical studies and demonstrate a device that works in a reliable manner," she says. This is how the COVID-19 breathalyser at OSU was developed, she adds.
Consider Nanda's example. His lab has expensive GC-MS equipment, an effective method to separate and analyse VOCs. But his goal is a point-of-care (PoC) e-nose for TB. For this, he needs to collaborate with experts in material sciences, sensor design and algorithms. "Initially we thought it would be easy… But while it looks rosy from a distance, once we get into the intricacies, we realise this is a different world altogether." Nanda says he is in talks with the Kolkata-based Centre for Development of Advanced Computing (C-DAC) to design a prototype. C-DAC has an e-nose to assess tea quality.
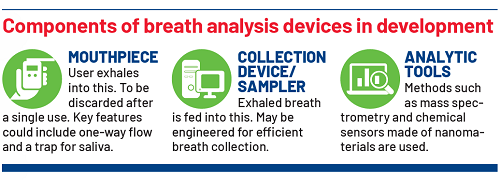
A PoC testing device must be small and portable with sensing elements that are effective and disposable, says Nair, whose company deals with PoC solutions. "This puts a lot more technological constraints on the problem." He explains that lab-based MS, while naturally suited for breath-testing, is not rugged and needs trained staff and a power source.
Molbio is considering amplifying fluorescent polymers (AFPs), or sensors with enhanced sensitivity, in an e-nose. An off-shoot of this research is Beaglez, Molbio's handheld detector for explosives such as RDX and TNT developed in collaboration with IIT Bombay. The question, says Nair, is how to make the sensors selective for different compounds so as to increase the breadth of detection.
At Technion, Haick has added an AI layer to the e-nose sensors. The AI Nanoarray has been able to detect more than 23 disease states such as cancers, liver and kidney ailments and pulmonary hypertension through exhaled breath in various studies. The AI nanosensors and algorithms were trained to recognise patterns or breath prints on samples of diseased and healthy patients.
Rapid breath tests for COVID-19 that offer hope for mass screening
Breathonix
(spin-off from the National University of Singapore)
How it works
- Breath is collected and fed* via sampler into a portable mass spectrometer
- Machine learning algorithm analyses sample and generates result
Status Provisional approval to test alongside rapid antigen tests (RATs) at checkpoints
Breathomix
(formed by a research group from the Amsterdam University Medical Center)
How it works
- Breath is fed* into the SpiroNose**
- Nose has 7 metal oxide semiconductor sensors for detection
- Cloud-based AI gives real-time result
Status Deployed commercially
NaNose Medical
(Technology developed by Technion-Israel Institute of Technology)
How it works
- Breath is fed* into breathalyser
- Proprietary smart sensor array measures VOCs***
- AI algorithm analyses pattern
Status Exploratory study in Wuhan in March 2020 showed high accuracy. Further validation needed
The Ohio State University
How it works
- Breath is fed* into a breathalyser
- Ceramic sensors specific to biomarkers generate change in electrical resistance
- Sensor output is a breath print specific to COVID-19
- Change is measured for a reading
Status Pending Emergency Use Authorisation by the U.S. FDA
*Exhaled breath via disposable mouthpieces.
** Integrates routine spirometry with electronic nose technology.
***Volatile organic compounds in exhaled breath.
Source: Company/researcher websites
For the IITR team, a simple colorimetric test seemed the most likely solution. Lahiri explains that an e-nose would require multiple inputs such as a sensing element, specific circuitry to support sensing, perhaps quantification of results in values on a reader and so on. This would increase the cost and the time to develop and defeat the purpose of an ‘anyone, anywhere' test.
LOOKING AHEAD
Despite the hurdles, a future for breath-based testing is within sight. The use of Big Data and machine learning to speed up biomarker discovery and pattern recognition is on the rise. Some COVID-19 breath tests such as one by the Netherlands-based Breathomix use AI and cloud computing for a real-time analysis; breath profiles are compared to an online reference database and analysed by machine learning algorithms. Agrawal of CSIR-IGIB says that there is agreement that Big Data and AI are critical for success. "But we are not at the phase where datasets are large or diverse enough to come out with a reliable solution yet." Efforts such as the centre of excellence should help generate more India-specific data.
For scientists and companies in India, there are challenges such as the relatively weak academia-industry linkages and inadequate risk funding.
Big Data of exhaled breath gas composition would be needed to fulfil the "ultimate goal" of testing exhaled breath for several diseases on one set of equipment, Zheng says. He adds that a "big leap" on such testing is possible if scientists from materials science, neural networks and respiratory medicine work together. Haick, whose AI Nanoarray has also been tested in COVID-19, says that with some modification to the AI, it can potentially serve as a diagnostic tool in case of a new disease outbreak.
As more companies get interested in the commercial potential of breath analysis, they will look for ways to monetise the technology. In the U.K., Owlstone Medical, an early mover in breath test development, is earning revenues from its breath collection and analysis products; customers include biomarker researchers and pharmaceutical companies pursuing precision medicine. "We are at an interesting cusp," Owlstone founder Billy Boyle had said in a 2019 podcast. "The technology platform now exists, and we are asking where it can be applied."
At IITR, Lahiri says that the team is in contact with industry partners – of whom one is keen to take this technology to market after clinical trials and regulatory certification. For scientists and companies in India, there are additional challenges such as the relatively weaker academia-industry linkages and inadequate risk funding.
While the last decade or more has seen an innovation ecosystem emerge, it is still a work in progress. Government funding for diagnostics start-ups is competitive and likely to go to solutions that can make a big impact with a relatively short gestation.
But it is important that the purveyors of breath analysis stay the course. Given the diverse factors that influence breath, a breath test may have to be specific to a population and/or geography. "You may not be able to take something standardised in (another country) and expect it to work," Balganesh says. If India has to benefit from a solution that checks many boxes at the same time, it will have to invest in building it.
(Overseas researchers were interviewed over e-mail.)
Have a
story idea?
Tell us.
Do you have a recent research paper or an idea for a science/technology-themed article that you'd like to tell us about?
GET IN TOUCH














