Messengers on a life-saving mission
-
- from Shaastra :: vol 01 edition 01 :: May - Jun 2021

Two scientists, across continents, collaborated to bring the mRNA vaccine to India. The technology, adapted for COVID-19 times, could open up new opportunities to treat other killer diseases.
STEVE REED first heard about Sanjay Singh more than a decade ago, when he went to the National Institute of Health (NIH) in the U.S., searching for people with expertise in manufacturing in India. Reed, an immunologist and a microbiologist, was interested in tropical infectious diseases, and had been working on developing vaccines against leprosy and leishmaniasis. He had expertise in vaccine adjuvants, a closely guarded technology in the pharmaceutical industry. He had worked at the NIH himself and wanted a business partner with matching interests and some expertise in manufacturing. “(Singh) was a famous guy in NIH,” says Reed. “I wanted someone to make things in India.”
Sanjay Singh had worked at the NIH in Washington, D.C., for six years before he decided to return to India in 2006. He had done his PhD on malaria biochemistry at the Central Drug Research Institute (CDRI) in Lucknow, and had worked on recombinant DNA technology at the International Centre for Genetic Engineering and Biotechnology (ICGEB) in Delhi before moving to the NIH. He had returned to Pune to set up a company called Gennova as a subsidiary of the pharmaceutical company Emcure. Gennova had started its business by making drugs for cardiovascular diseases, but Singh had retained his original interest in malaria and other tropical diseases.
A decade ago, after Reed called Singh, their interests converged quickly in a business partnership. In 2019, Reed co-founded a company called HDT Bio in Seattle for developing messenger RNA (mRNA) technology for cancer treatment. When the COVID-19 pandemic hit China, Reed immediately started tweaking the technology to develop mRNA vaccines against the virus. Singh, sensing that the battle against the pandemic would be long and hard, approached the Department of Biotechnology (DBT) for seed money to develop an mRNA vaccine.
Traditional vaccines require large facilities for culturing microorganisms or cells; mRNA vaccines can be made in a small facility, and are easy to tweak for emerging mutations.
Reed is now trying to do clinical trials in South Korea, China, and some African countries for the HDT-301 vaccine. In April this year, Gennova started clinical trials for a modified product, called HGC019, providing the country with a potential tool to control the pandemic in the long term: an inexpensive vaccine that can be quickly tweaked, manufactured, and then distributed rapidly around the country. The businesses of Reed and Singh had converged unexpectedly to their original interests. HDT Bio had generated the initial discovery, and Gennova had improved the product and the manufacturing technology.
A RADICAL IDEA
The idea of using mRNA for vaccines was born in the early 1990s. Katalin Kariko, a biologist at the University of Pennsylvania, had made the first grant application in 1990 to develop the technology. However, it was too radical an idea for funding agencies, and no one was willing to fund it, primarily because there was no way of injecting mRNA into the body without the immune system mounting a response against the vaccine itself. The solution was found more than a decade later by Kariko and her colleague Drew Weissman. They tweaked the part of the mRNA that was alerting the immune system and developed a way of getting mRNA into the cells.
With this crucial breakthrough, mRNA technology was ready to be developed as a therapy for a number of diseases. A major landmark came in 2012 with the founding of Moderna in Boston as a vaccine company. In 2013, Kariko joined a German immunotherapy start-up called BioNTech and helped the company’s journey towards mRNA technology. mRNA vaccines were under development in BioNTech and Moderna when COVID-19 struck. A serious pandemic was a good opportunity to try a new technology. BioNTech formed a partnership with Pfizer, and Moderna went alone. Both vaccines were launched in 2020. It was a small first step for the world.
Even before the product was launched, the drawbacks of the mRNA vaccine were evident. Messenger RNA degrades very rapidly and is therefore difficult to store and transport. The vaccine of Pfizer-BioNTech is stored at minus 70º Celsius, which is difficult to maintain in most countries. On the other hand, the Moderna vaccine can be stored at between 2º and 8º Celsius for a month, a substantial improvement over the Pfizer vaccine. HDT-301 can be stored as a liquid for two months at minus 20º Celsius, but Gennova has improved it for storage between 2º and 8º Celsius for two months. The original HDT vaccine can also be dried as a powder and stored at room temperature for long periods.

THE UPSIDE
In spite of the storage difficulties, mRNA vaccines bring substantial benefits. For one thing, they are easy to make and tweak. Traditional vaccines require large facilities for culturing micro-organisms or cells, while mRNA vaccines can be made in a small facility. Since mRNA is synthetic, there is no risk of contamination from live cells or viruses or bacteria. The mRNA vaccine can be made very quickly, and it can also be tweaked for emerging mutations rapidly. “The technology is so advanced that you can start in the morning, and by evening your vaccine is ready,” says Singh. If scientists spot a mutation in a virus, a new mRNA vaccine can be developed in two months.
All mRNA vaccines provide these benefits. The HDT-Gennova vaccine has additional features that make it even more useful. It is self-amplifying, which means that it can be given in small doses. For example, while current mRNA vaccines are given at doses between 30 and 100 micrograms, the Gennova vaccine may be given at less than 5 micrograms. The lower dose has a big impact on manufacturing and price; a reactor that makes self-amplifying RNA can make 50-100 times more doses with the same reactor size.
Gennova has made some important changes to the original HDT-301 vaccine. HDT had made the vaccine in two vials, one the dried mRNA and the other a substance called a diluent, whose function is to reconstitute the vaccine for clinical use. Gennova’s HGC019 is made in one vial. The diluent has a lipid-based nanoparticle emulsion (LION) that is being tested for the first time, and so Gennova had to do separate animal trials for LION and the vaccine. Over the next few months, the speed of its progress will depend on how closely the results match that of the other mRNA vaccines.
The HDT-Gennova partnership brought mRNA technology into the country in the nick of time, but its future is not restricted to vaccines for COVID. Reed and Singh are planning to use it for cancer therapy sometime in the future, and their favourite area of infectious diseases. The technology will be developed for vaccinating against a number of infectious diseases like seasonal flu, malaria, dengue, West Nile virus, and so on. In fact, scientists at Yale University are already working on an mRNA vaccine for malaria, also using self-amplifying technology.
Gennova has the capacity to make 100 million doses of the COVID vaccine after approval. Singh is planning to ramp up capacity to vaccinate the entire country.
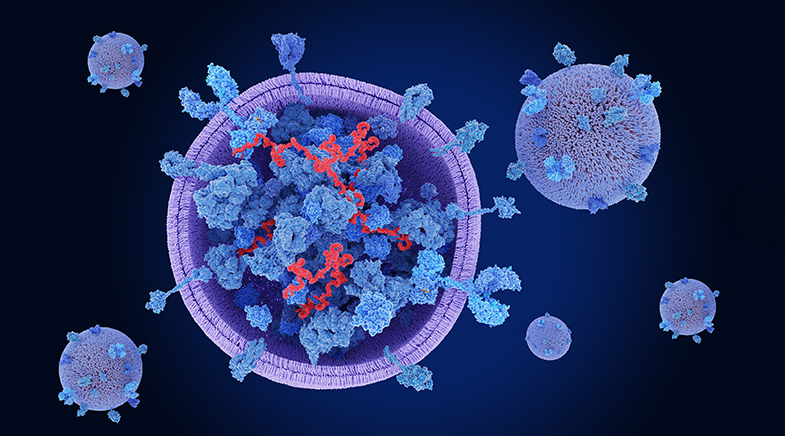
The mechanics of mRNA
Making a protein is a bit like making a dish using a recipe. And yet it is different from cooking in that the recipe is stored safely somewhere and cannot be accessed by the chef directly. A messenger, called messenger RNA (mRNA), carries the information to make the protein – the sequence of amino acids – from the nucleus of the cell to the cytoplasm where proteins are made. Once the protein is made, the mRNA degrades.
This elegant machinery makes sure that the blueprint for protein synthesis is not tampered with, and can be passed on from generation to generation without change, other than mutations that happen occasionally. In principle, it also gives scientists a method to make easily any protein that the body needs. Make an mRNA and put it inside the cell, and you could coax it to make the corresponding protein.
In the last decade, biologists learned to synthesise mRNA of any sequence in the laboratory and developed methods to carry it safely inside the cell. It is now relatively easy to make mRNA in the laboratory but not so easy to carry it safely inside the cell without degradation. Since mRNA degrades easily, it has to be attached to a larger molecule or wrapped inside a vesicle for delivery. It is also important that the immune system does not recognise mRNA as an intruder and start attacking it.
The development of mRNA has far-reaching consequences for dealing with future pandemics, but there is still a lot that we do not understand. The long-term side-effects of mRNA vaccines are likely to be small, since mRNA degrades rapidly, but data need to come from actual patients over a number of years. Scientists also would need to see how long an immune response will last. For the moment, they are largely optimistic.
Have a
story idea?
Tell us.
Do you have a recent research paper or an idea for a science/technology-themed article that you'd like to tell us about?
GET IN TOUCH