To the point
-
- from Shaastra :: vol 01 edition 03 :: Sep - Oct 2021
The study of exhaled breath could aid the cause of precision medicine.
Why do some people respond better than others to a given treatment, and why do some experience more severe side effects? Modern medicine continues to grapple with such questions, especially for complex diseases. Precision medicine is an emerging approach that looks into factors such as genomics, environment and lifestyle that could impact a patient's response to treatment. It seeks to refine and customise therapy for smaller sub-groups rather than look for treatments that work for the average patient.
Research suggests that studying exhaled breath could aid the cause of precision medicine. In 2017, in a study in the Journal of Translational Medicine, a team at the All India Institute of Medical Sciences (AIIMS) and the Council of Scientific & Industrial Research-run Institute of Genomics and Integrative Biology (CSIR-IGIB) could group asthma patients into three types based on the metabolites identified in their exhaled breath condensate (aerosols in exhaled breath from the lungs' lining fluids that are condensed for analysis). These groups were found to differ clinically as well.
Studies such as this prompted the Indian Council of Medical Research (ICMR) to fund a centre of excellence for breathomics just before the pandemic. The focus is on respiratory diseases such as asthma and Chronic Obstructive Pulmonary Disorder (COPD). The centre will experiment with various techniques for breath analysis.
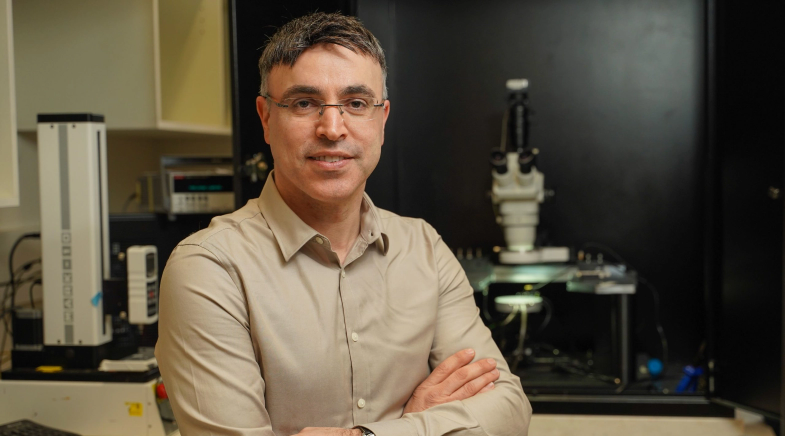
It has two objectives, says Anurag Agrawal, Director, CSIR-IGIB, and a co-investigator. One is breath-based diagnostics. The other is precision medicine or gauging "who is likely to respond well to a therapy, and who is not."
Breath analysis that could reliably identify sub-types and help match patients and treatment would be a game-changer. For instance, while elevated nitric oxide level is globally an accepted biomarker for asthma, a study in an Indian paediatric cohort by researchers including Agrawal found it had little clinical value in diagnosing or predicting severity in a cohort of children with asthma.
Going forward, research needs to be scaled up. "You need large numbers to be followed regularly," Agrawal says. That is a key reason why the centre is located in AIIMS, a public tertiary care hospital.
Breath analysis that could reliably identify sub-types and help match patients and treatment would be a game-changer.
At IIT Madras, fluid dynamics experts are studying the flow velocity of exhaled breath to identify so-called turbulence signatures that could indirectly help improve the effectiveness of inhaled drugs. Exhaled breath is pushed out by the lungs through the extra-thoracic region (ETR) – the portion between the nose and lungs, including the nasal and oral passages, pharynx and larynx. The physical characteristics (so-called morphological structures) of the ETR vary from person to person.
Researchers at the IIT Madras hypothesised that these physical differences could impact breath 'turbulence' or how exhaled breath moved through the ETR. And, further, that it is possible to identify unique turbulence signatures that could help classify humans. A preliminary study, which also employed machine learning, on 94 volunteers showed this approach to be promising, according to Mahesh Panchagnula, Professor of Applied Mechanics, IIT Madras, and a co-author of the study being prepared for publication.
The finding can have two possible uses: one, exhaled breath turbulence signature as a unique ID like the fingerprint or iris. Two, it may be used to infer the geometry of the ETR. The latter may make inhalation therapy for diseases such as asthma more effective. "In the case of inhaled drugs, not all of it is delivered to the lungs," explains Panchagnula. A portion is trapped in the ETR, impacting drug effectiveness. If doctors could measure this loss, they could recalibrate dosing to make up for it. But it differs from patient to patient, he points out.
Panchagnula's department is collaborating with the Sri Venkateswara Institute of Medical Sciences, Tirupati, to better understand interpersonal variations in pulmonological functions. In joint experiments, they have demonstrated how the presence of radio-labelled inhaled aerosols in the lungs of volunteers differed from one subject to another. This is where inferring the geometry of the ETR helps. This knowledge could be used to classify patients into smaller groups and their inhalation therapy dosage optimised accordingly.
Progress in breath-sensing methods too could aid precision medicine. For instance, at the Technion - Israel Institute of Technology, an AI-enabled breathalyser was able to classify three sub-types of gastric cancer patients in a large screening population of healthy and diseased, with 100% sensitivity and 87% specificity, says its inventor Hossam Haick, Full Professor, Department of Chemical Engineering. It was also able to discriminate between volatile organic compounds associated with genetic mutations in certain diseases such as the K-RAS and EGFR genes in cancers. This could help in personalised diagnoses and treatment, Haick says.
Have a
story idea?
Tell us.
Do you have a recent research paper or an idea for a science/technology-themed article that you'd like to tell us about?
GET IN TOUCH