Repeat offenders
-
- from Shaastra :: vol 04 issue 03 :: Apr 2025

A rare 'gift' points the path to therapies for a genetic disorder.
Some 120 fragments of a human brain frozen to –80° Celsius lie sealed in tiny containers in a brain repository in Bengaluru. They belonged to a man whose family gifted his brain to science upon his death in 2015, shortly after his 84th birthday. For over 40 years, he had battled spinocerebellar ataxia-12 (SCA12), a rare, slow-progressing brain disorder that causes tremors in the arms and head, and balance and speech difficulties.
SCA12 is an inherited genetic disorder that, for reasons still unclear, is disproportionately common in India, particularly among the Agarwal community. While brain imaging scans offer limited insights into such disorders, direct studies of brain tissues can reveal what has gone wrong at the cellular level. Among the 300 brains in the repository at the National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru, only one is from an SCA12 patient; it promises a rare glimpse into an understudied disease.
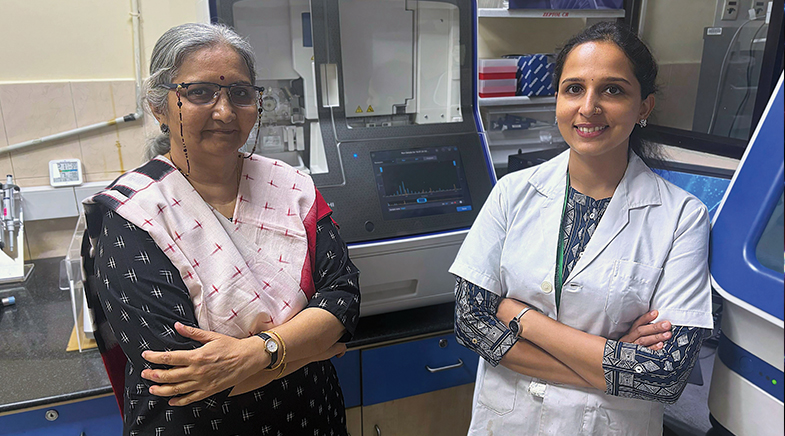
Now, NIMHANS researchers have conducted the first cellular-level analysis of an SCA12 brain, uncovering fresh clues about how the disorder unfolds and revealing potential pathways towards designing therapies against SCA12. Like several other genetic disorders, SCA12 strikes in middle age, typically in a person's 40s. "The goal of therapy would be to delay or block the mechanisms that trigger the disease," says Meera Purushottam, a medical geneticist at NIMHANS who led the study on the SCA12 brain (bit.ly/brain-sca12).
SCA12 belongs to a group of some 30 genetic disorders caused by abnormally large counts of so-called triplet repeats and hitherto considered incurable. The backbone of DNA, the genetic material, is made up of a long string of molecules called nucleotide bases: adenine (A), cytosine (C), guanine (G), and thymine (T). In certain segments of the genome, some combination of three of these four bases form repeating triplets such as CAG CAG CAG or CGG CGG CGG or CTG CTG CTG; when this is expanded to abnormal numbers, it leads to the disease.
Like several other genetic disorders, SCA12 strikes in middle age, typically in a person's 40s.
In 1991, a team led by American geneticist Stephen Warren at Emory University discovered that an abnormally high count of CGG repeats in a gene named FMR1 causes Fragile X syndrome (FXS), a disorder with intellectual and behavioural symptoms. In people without FXS, the FMR1 gene has five to 44 CGG repeats. In patients with FXS, the gene contains 200 or more CGG repeats.
Through the 1990s, scientists found more genetic disorders with triplet repeat expansions. People who have 40 or more CAG repeats in a gene known as huntingtin develop the particularly severe and life-shortening Huntington's disease which also strikes in middle age. Healthy people have 35 or fewer CAG repeats in the huntingtin gene. And patients with SCA12 have 50 or more CAG repeats in a gene called PPP2R2B, while healthy people have seven to 28 CAG repeats in that gene.
HIGH PREVALENCE
Genetic studies over the past two decades suggest that the vast majority of SCA12 patients in India are from the Agarwal community, with some research indicating up to 80% prevalence within this group. In 2005, a research team at the Institute of Genomics and Integrative Biology in New Delhi attributed this pattern to the "founder effect" – a genetic phenomenon where a mutation introduced generations ago by an individual or a few individuals gradually spreads through a population. The IGIB researchers who analysed the genetic make-up of SCA12 patients at the All India Institute of Medical Sciences, New Delhi, detected evidence for at least two such introductions.
While SCA12 prevalence in non-Agarwal communities is low, researchers say it is clinically relevant because it is not uncommon for doctors to rule out SCA12 when the patient is from a non-Agarwal community. Doctors should be aware that members of non-Agarwal communities may also develop SCA12 either through the emergence of novel mutations or more commonly through ancestral migrations, population intermixing, or intercommunity marriages, a NIMHANS team had cautioned in a study in 2022 (bit.ly/sca12-agarwal).
SCA12 is marked by the loss of neurons, or brain cells, in the cerebellum, a brain region that coordinates movement and balance, among other tasks. The cerebellum accounts for only about 10% of the brain's volume but holds over 50% of its neurons, its high density of cells underscoring its critical role in motor control and cognitive functions.
Meera and her colleagues estimated CAG repeats in the PPP2R2B gene and measured the gene's activity in different regions of the brain from the SCA12 patient. They discovered that cells in different regions of the brain had varying genetic make-up. "This challenges the traditional idea that all cells in an organism have the exact same genetic make-up all the time," says Meera. The number of CAG repeats was not uniform across the brain – some regions had much higher repeat counts than others. Paradoxically, the cerebellum – the brain region most affected by SCA12 – had the lowest counts of the CAG repeats.
SURVIVORSHIP BIAS
Meera speculates that the paradox could be the outcome of what is known as "survivorship bias" – an error that emerges from observations based on only survivors, while disregarding those that failed or were eliminated.
"Similarly, what we're seeing are the cells in the cerebellum that had survived; it is possible that cells with large triplet expansions have perished and are no longer available for observations," says Meera. The scientists also found that the PPP2R2B gene was significantly less active in the cerebellum samples of the SCA12 patient than in the repository's samples from healthy individuals who had died in road accidents.
Collectively, the findings suggest that the expansion of CAG repeats in the PPP2R2B gene is a slow, selective process occurring over years and that the disease strikes when the CAG repeats exceed certain thresholds.
"The accumulation of CAG repeats is a slow process," says Sanjeev Jain, Emeritus Professor of Psychiatry and scientist in the Molecular Genetics Laboratory at NIMHANS and co-author of the March 2025 study. "It therefore allows us a window of opportunity to try to regulate or modify the mechanism driving that process."
A THERAPEUTIC STRATEGY
The broad therapeutic strategy would seek to prevent the accumulation of additional CAG repeats on the PPP2R2B gene. One option would be to enhance the activity of DNA modifier genes involved in repairing DNA mismatches or errors that lead to additional CAG repeats. These DNA mismatch repair genes work like spell-checkers for DNA, correcting errors before they accumulate.
Research groups elsewhere have already begun exploring such strategies against Huntington's disease. Neuroscientist Gillian Bates and her team at University College London, for instance, have shown through experiments on lab mice that blocking a gene called MSH3, which helps fix DNA errors, can stop the CAG repeats from expanding in the brain.
REPAIRING A MISMATCH
Another study on mice led by neurobiologist X. William Yang at the University of California, Los Angeles, has suggested that a specific subset of DNA mismatch repair genes drives Huntington's disease in vulnerable neurons where they lead to rapid expansion of CAG repeats. The UCLA researchers tested six DNA mismatch repair genes and found that two – MSH3 and PMS1 – strongly impacted the disease process.
Their results, published in the journal Cell, suggest that reducing the activity levels of MSH3 and PMS1 could be a potential therapeutic strategy against Huntington's disease. The study showed that targeting MSH3 can alleviate motor and gait deficits and improve neuronal protein levels in the mice. "We were surprised to see the potent and sustained effects of targeting these mismatch repair genes in these mice – the benefit lasts up to 20 months of age in the mouse, which would be comparable to about 60 years in humans," says Yang. "Our study suggests that these genes are not just disease modifiers... but are genetic drivers of Huntington's disease."
Efforts to manipulate DNA mismatch repair genes have already translated into clinical applications in cancer. For instance, drug regulatory authorities have approved molecules known as Poly (ADP-ribose) polymerase (PARP) inhibitors against breast, ovarian, and prostate cancers. Scientists are also evaluating other molecules and gene-editing strategies to tweak DNA repair genes and restore tumour suppression.
"The challenge is whether we could use such insights from oncology to develop new drugs for neurodegenerative disorders that have been considered incurable," says Jain. "This is an idea at present, but SCA12 is common in India and we probably have sufficient biotech expertise in the country to start working on such leads."
G.S. Mudur is a science journalist.
Have a
story idea?
Tell us.
Do you have a recent research paper or an idea for a science/technology-themed article that you'd like to tell us about?
GET IN TOUCH