Magnificent magnesium
-
- from Shaastra :: vol 03 issue 05 :: Jun 2024
Oh Mg! This new biomaterial is drawing the interest of researchers making medical implants.
For over a decade now at the Helmholtz-Zentrum Hereon, a research institution in Geesthacht, Germany, Regine Willumeit-Römer has devoted her time and energy for a singular cause: developing novel materials for biocompatible medical implants. In her latest research project, she directed her attention towards people with ailments such as bipolar disorder, exploring a biocompatible implant that would release lithium medication directly into the brain, instead of being administered orally. She needed the right carrier, and the answer lay in a metal she had been closely working with: magnesium.
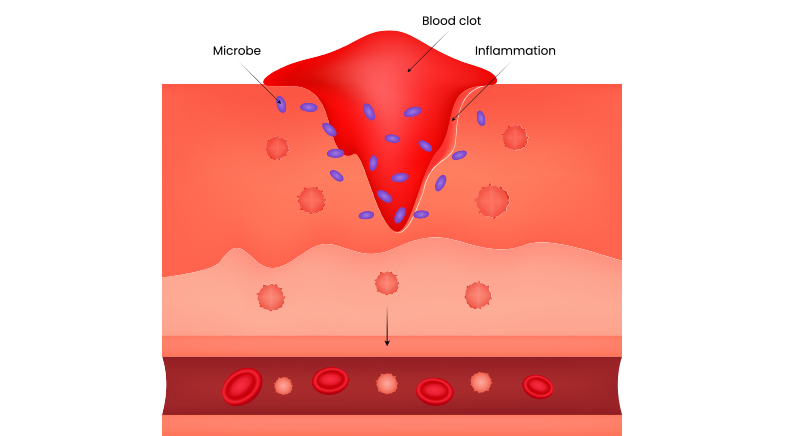
The metal, an important micronutrient in the human body, has captured the interest of medical device manufacturers because of its resorbability and anti-inflammatory properties. At the Hereon centre's Institute of Metallic Biomaterials, Willumeit-Römer was looking at magnesium alloys, which could break down inside a body over time, for orthopaedic and cardiovascular applications. She then went on to explore the neurological applications of magnesium alloys.
A biocompatible substrate can deliver a drug locally, and, in doing so, expose the body to lower amounts of lithium.
For this project, she enlisted Krathika Bhat, a bioprocess engineer who also co-authored a study (bit.ly/lithium-delivery), published in April 2024. Although lithium has long been used to treat bipolar disorder, it has a very narrow therapeutic range. The paper explains that it can produce beneficial effects only in a small concentration range in the blood. Beyond this range, lithium may lead to side effects such as tremors and nausea, and, in extreme cases, thyroid and renal dysfunctions.
"We traditionally take lithium orally and it has to circulate throughout the body via the blood before reaching the brain where it is meant to function. A lot of lithium is lost in the process and very little reaches the brain. We end up ingesting a lot of lithium before it reaches therapeutic levels in the brain to have the intended effect," Bhat says. The solution to this, the scientists concluded, would be a biocompatible substrate that could deliver the drug locally, and, in doing so, expose the body to lower amounts of lithium.
Bhat explains that a tablet when taken orally leads to a sudden spike in concentration as it is metabolised, with the level dropping over time. "But when we have a properly controlled drug release from a substrate or implant like this, it remains consistent at a lower level, and the side effects can be reduced," she says.
Willumeit-Römer and Bhat tested the implant in vitro — in a culture of glial cells present in the nervous system. They zeroed in on magnesium as the ideal substrate as they needed it to corrode at a specific rate to release the drug and allow cell adhesion to its surface.
At the time, Bhat was also working on a project to use magnesium in nerve regeneration at the University of Cincinnati in the U.S. "We used nerve guidance conduits to allow nerves to heal after they have been cut. We put this sort of bridge of magnesium that helps the nerve grow back and then, by the time the nerve is fully grown, the bridge is corroded and just the regrown nerve is left," Bhat says.
Companies such as MgShell, a spinoff of the Polytechnic University of Milan in Italy, are also experimenting with the use of magnesium in drug delivery systems, creating intraocular devices for retinal diseases such as macular degeneration. The device is designed to release drug doses at pre-set times, negating the need for multiple injections over the years. The company has patented its technology, which is undergoing pre-clinical validation.
"There is also some research around using magnesium as electrodes to record neuron activity in the brain. But none clinically approved yet," she says.
HEALING TOUCH
Magnesium, however, has already found its footing in the orthopaedic implant sector, with companies such as Syntellix in Germany creating magnesium alloys with rare-earth elements to produce screws, pins and plates that are equivalent to titanium implants.
When a bone fractures, the fragments need to be held together to allow it to heal. Traditionally, plates, screws and nails (or rods in the case of long bones), made of titanium and stainless steel, are used to hold the bone together. These implants stay in the body permanently, unless surgically removed later. A magnesium alloy implant will stay in the body until the bone has healed, and then be resorbed inside the body and transformed into bone tissue. Magnesium is even expected to help with bone growth.
"One big advantage of magnesium implants is that it is lightweight," says Chinmay Khare, Founder of Pune-based Wissenkraft Labs, which works on advanced materials technology. When alloyed with the right material, the alloy's Young's modulus value (an indicator of stiffness) is "very close" to that of the human bone, he says. The Young's modulus measure for stainless steel, on the other hand, is "way higher" than that of bones, he says. At Wissenkraft, Khare is developing a coating to combat the loosening of titanium implants over time due to bacterial infections. However, he doesn't yet work with magnesium coatings or implants. "We would be interested in it when the time is right," he says.

And that time may be here soon. According to Anishay Raj, Director of Exclusive Magnesium, providers of commercial magnesium alloys, queries for magnesium by researchers in the bioengineering field have grown from one query in six months to one every month or so in the past two years. "Mg-calcium, Mg-zinc and Mg-alloy ZE41 (containing zinc, zirconium and rare-earth elements) are receiving attention," Raj says.
Commercial products, however, are not yet available in India because it is a challenge to get the right alloy composition that would delay the corrosion rate of magnesium inside the body while not being toxic to humans, Khare says.

This challenge has been central to T.S. Sampath Kumar's work at the Indian Institute of Technology Madras. Professor Emeritus at the institute's Department of Metallurgical and Materials Engineering, he researches nanostructured biomaterials — in particular titanium and magnesium alloys — to create medical implants. He has collaborated with Uday Chakkingal, also a Professor in the department. "The problem we are trying to solve is that magnesium deteriorates rapidly in the human body," says Chakkingal. So, he points out, it may disappear even before it manages to hold the bone together. "The rapid degradation also means that the human excretory system has to be able to remove the extra ions produced. It can also lead to the evolution of hydrogen gas, so there is a risk of hydrogen gas blisters at the site of the implant."
Their team at IIT Madras, instead of experimenting with different alloy compositions to control the degradation, came up with a different solution to the problem. "We modified the microstructure of the magnesium alloy such that the surface of the alloy would react to the biofluids in a slower fashion," Sampath Kumar says. They have patented this technology.
A magnesium alloy implant will stay in the body until the bone has healed, and then be resorbed inside the body.
To achieve this, they worked with their student, Manas Ranjan Sahu, now a research scholar at the National Institute for Materials Science in Japan. The team pressed the alloy alternately between grooved and flat die-casts to deform it uniformly. This caused the coarse grains (or crystals) on the surface to break down into finer ones. The more the number of grains, the greater the grain boundary area. "These boundaries are high-energy areas that attract the deposition of calcium phosphate from the plasma. These deposits on the implant control its rapid degradation," Sahu explains. In orthopaedic applications, the implant needs to last 12-24 months to be effective, while in cardiovascular stent applications, it needs 6-12 months.
As the research around magnesium develops further, industry giants are taking note. Chakkingal has been working with Tata Steel, which is interested in venturing into magnesium medical implants. They are jointly developing fracture fixation implants — the process is likely to take at least 2-3 years, Chakkingal reckons — and will explore filing a patent for it.
Have a
story idea?
Tell us.
Do you have a recent research paper or an idea for a science/technology-themed article that you'd like to tell us about?
GET IN TOUCH