Psychedelic pacifiers
-
- from Shaastra :: vol 03 issue 09 :: Oct 2024
Researchers identify a tiny brain region responsible for reducing anxiety in mice.
Praachi Tiwari vividly remembers a random discussion she had with her doctoral advisor and neurobiologist, Vidita Vaidya, five years ago at the verdant campus of the Tata Institute of Fundamental Research (TIFR) in Mumbai. The discussion veered around serotonin, a key neurotransmitter (a chemical that aids communication between neurons) in the brain, and its role in triggering anxiety response, which became Tiwari's PhD topic.
The work unravelled a neural circuit that channels the therapeutic effect of a psychedelic; it also identified receptors that induce the effect.
Tiwari, currently a post-doc at the Center for Psychedelics and Consciousness Research at the Johns Hopkins University School of Medicine in the U.S., along with Vaidya, Professor at TIFR, and co-workers, have achieved something profound. Through extensive work on the brains of mice and rats, they have identified a tiny brain region responsible for reducing anxiety-like behaviour when a psychedelic is administered. Psychedelics, such as the drug LSD, are substances that trigger hallucinations and altered states of consciousness. Their use is banned in most countries.
NEW CLASS OF DRUGS
The work, which appeared in the journal Neuron (bit.ly/Vidita-Neuron) in September, not only unravelled a neural circuit that exclusively channels the therapeutic effect of a psychedelic drug but also identified a small population of receptors responsible for the beneficial effect. The discovery of the receptors prompted the team to go to the next step. They show that the same response can be elicited even without the psychedelic if they can activate the neurons involved through other chemical entities, opening up avenues for a new class of psychedelic-inspired drugs.
The results come at a time of an increasing realisation of the promise that psychedelics hold in treating many neuropsychiatric conditions, particularly those resistant to existing therapies. As many as seven psychedelics, including psilocybin – the psychoactive ingredient found in magic mushrooms – are being studied in more than 200 trials currently.
For the study, the scientists used a synthetic psychedelic drug with the formula 2,5-Dimethoxy-4-iodoamphetamine or DOI, first synthesised by late U.S. biochemist Alexander Shulgin in 1984. Like many other psychedelic drugs, DOI has a high affinity for serotonin receptors in the brain.
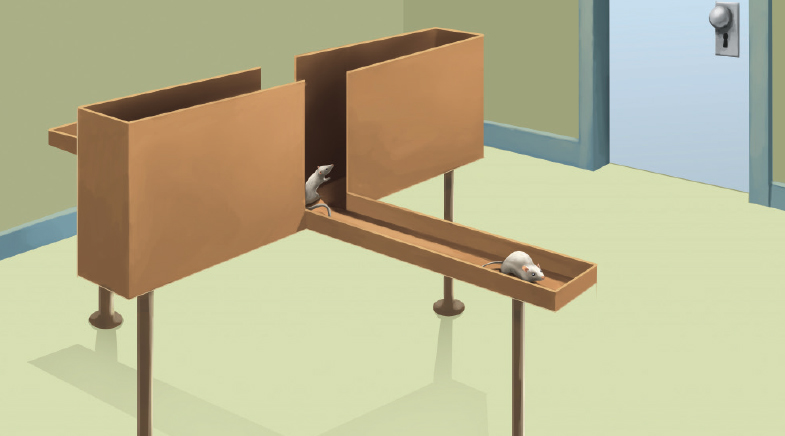
To begin with, the researchers confirmed that the psychedelic has an anxiety-lowering property, something that was reported earlier. The team tested this using an apparatus called elevated plus maze, which is used in labs for measuring anxiety. The tool, which stands 2 feet from the ground, has two open and two closed arms with high walls on three sides. When their anxiety levels were low, the rodents, which normally prefer to stay in closed arms, ventured out and spent considerable time on exposed open arms.
However, the part of the brain responsible for this anxiety-lowering behaviour upon DOI administration was still not known.
To identify the brain region, the researchers targeted serotonin receptors in brain regions that were previously known to be associated with anxiety one by one, including the prefrontal cortex (PFC), amygdala and hippocampus (ventral and dorsal). For this, they surgically cannulated the animals in such a way that they could infuse the drug only to the desired part of the brain. Much to their surprise, the researchers found that it was not the regions where serotonin 2A receptors are abundantly present, such as PFC, that were responsible for the anxiety reduction effect, but the ventral hippocampus, where their population was abysmally small. "It was not our main...suspect, but we chose that region because it was earlier implicated in anxiety," says Vaidya.
To be doubly sure, the scientists then blocked these serotonin 2A receptors in the ventral hippocampus in some animals and administered the drug to their brains, which understandably showed no effect on anxiety, while they exhibited hallucinatory behaviour by way of head-twitching. "This showed that the receptors in this part are not just important but absolutely essential for the drug to have an effect on anxiety," she explains.
COLLABORATIVE SCIENCE
"The work by the Vaidya Lab is significant because it uncovers the specific brain region and cell types that are essential for driving psychedelic's effects on anxiety...this is the best example I know where research was able to pinpoint exactly where the drug is acting in the brain that lead to the behavioural changes," says Alex Kwan, Associate Professor of Biomedical Engineering at Cornell University, who has been studying the effects of psilocybin on depression and post-traumatic stress disorder (PTSD).
In separate work done on mice (bit.ly/Psilocybin-Kwan), Kwan and his team recently showed how psilocybin can have beneficial effects on a certain type of therapy, called prolonged exposure (PE) therapy, in PTSD patients. A cognitive behavioural therapy, PE primes a patient to gradually approach trauma-related memories, feelings and situations that they have been avoiding since the trauma. "Our results show that psilocybin may provide benefits because it can accelerate extinction, which if true for humans, would help alleviate the PTSD symptoms," says Kwan, a skilled neuro-electrophysiologist.
Kwan is also a co-author of the Neuron study. He and his MD-PhD student Pasha Davoudian helped Tiwari and Vaidya identify the neuron cell type – a class of fast-spiking interneurons, called parvalbumin interneurons – in the ventral hippocampus whose firing goes up under the influence of DOI.

Identifying the neuron cell type and establishing these neurons' connection with the serotonin receptors that were seen to reduce anxiety opened a world of possibilities before Tiwari and Vaidya. Using knockout mice, they successfully restored serotonin 2A receptors only on parvalbumin interneurons and found that the anxiety-reducing property of the drug was still there but without any undesirable hallucinatory behaviour.
"Then Praachi had a better idea," says Vaidya. "If this is conceptually true, if one can switch on the firing of these cells, the animal can show less anxiety. So, using a chemogenetic tool (a genetically engineered system that allows for precise control of specific cell population using a chemical ligand), she showed that the firing of these neurons can be increased," she explains.
"My engineering background gave me the confidence to build new things, sometimes new equipment and sometimes an experimental approach. Especially with neural circuits, it felt second nature to me when I tried to visualise connections and structures in the brain," adds Tiwari.
Whenever drugs inspired by psychedelics come to market, those who fail to respond to existing medication will benefit the most.
By revealing the underlying mechanism of action of a potential drug inspired by a psychedelic, the work can boost research into psychedelic drugs. It follows the U.S. Food and Drug Administration's controversial decision to decline the approval of MDMA as a treatment for PTSD.
A recent editorial in Science (bit.ly/Psychedelic-Edit) highlighted the need for unravelling neural pathways through which psychedelics work, little of which is currently known. "Identifying mechanisms underlying neurobiological changes, alterations in consciousness, and shifts in emotional and cognitive processes should provide critical insights into how and why these compounds and PAT (psychedelic-assisted therapy) work," it said.
If and when these psychedelic-inspired drugs hit the clinics, major beneficiaries would be those who currently fail to respond to existing medications, who are in sizeable numbers.
"In clinical settings for anxiety and depression, the biggest challenge is that the medications need 6-8 weeks for their clinical action, and that about 50% of patients need many medication trials with high chance of treatment resistance. Hence, there is a need to discover rapidly acting agents," says Biju Viswanath, Associate Professor of Psychiatry at the Bengaluru-based National Institute of Mental Health and Neurosciences (NIMHANS).
"The study by Vaidya and others provides key insights to understand the mechanisms of rapidly acting serotonergic psychedelics. Interestingly, they have mechanistic findings in the hippocampus, which is a well-established brain region affected in major depression, enhancing the relevance of this study," says Viswanath, who was not involved in the work.
Have a
story idea?
Tell us.
Do you have a recent research paper or an idea for a science/technology-themed article that you'd like to tell us about?
GET IN TOUCH