Proton therapy: the beam of hope
-
- from Shaastra :: vol 03 issue 01 :: Jan - Feb 2024

A new centre harnesses high-energy proton beams to transform the way certain cancers are treated.
The dark clouds had the team of doctors worried. It was monsoon time in Mumbai, and the cyclotron — a particle accelerator crucial for a revolutionary treatment of cancer — needed to be put in place before the season's first downpour. For this, a room of a particular size had to be readied, keeping humidity and temperature under strict control. And it had to be sealed from the top with concrete.
As it happened, it started to rain only after the cyclotron had been brought to Mumbai and erected, and the roof had been sealed. The centre with the cyclotron — in Navi Mumbai's Kharghar, a few miles from bustling Mumbai — is a facility that promises to revolutionise the way cancer is treated in the country.
The Tata Memorial Hospital's Advanced Centre for Treatment, Research and Education in Cancer (ACTREC), India's first proton treatment centre that offers free treatment for the poor, is ready. Ten years after the idea of such a facility was mooted, therapy for the first group of patients started in August 2023.
Unlike traditional radiation therapy, protons can be modulated to deliver a high radiation dose to a tumour while sparing healthy tissues.
Proton therapy, or proton beam therapy, is a type of radiation that uses high-energy beams of protons to target and destroy cancerous cells. Unlike traditional radiation therapy, which uses X-rays, protons can be modulated to deliver a high radiation dose to a tumour while sparing the surrounding healthy tissues. X-rays are lighter and get scattered; protons are heavier — the beam spreads less radiation to the surrounding cells on its path to the tumour and deposits the maximum energy on the cell.
However, managing protons is far more challenging than working with X-rays. A proton centre is considered the world's most expensive and complex medical device for treating cancer. Building its parts is akin to building a nuclear weapon: it calls for an accelerator that speeds up the nuclear particle to the speed of light, ways to control its shooting into tumours, and bunkers to protect everyone involved from the radiation. The high construction cost also puts it out of reach of the masses.
FROM BEAMLINES TO GANTRIES
ACTREC in Kharghar is a giant monument rising out of an urban jumble. The three-storey facility was built over an acre of land because proton beams must travel horizontally on a level plain to attain high energy. The centre, built at a cost of `1,000 crore, was in the works for almost a decade. Giant machines were procured from overseas and installed. Most of the work happened during the pandemic, putting enormous pressure on its planners, points out Dr Siddhartha Laskar of the Department of Radiation Oncology at the Tata Memorial Hospital (TMH). Laskar, who is in charge of proton therapy at the hospital, has been involved in the planning and development of ACTREC from the very beginning.
The idea to bring proton therapy to the hospital took shape after he and his colleagues realised the need for a more precise and effective form of radiation therapy. "When we started thinking about this, we had no experience," he says. "Nobody was giving us the technical specifications. We had to find out from various sources the best way to go ahead with this." Laskar's team proposed a three-room facility to the Atomic Energy Commission, which funds the hospital, and got the go-ahead in 2014.
At the heart of the system is the cyclotron, a massive steel magnet that accelerates protons to high energies. The protons need to be accelerated to 230 mega electron volts (MeV) of energy after being extracted from a hydrogen arc. "That is why you need a cyclotron," Laskar says. "Otherwise, it will not penetrate the body in depth."
The protons are then directed to the tumour through channels called beamlines and into gantries in the treatment room. "The entire system is computer-controlled," Laskar explains. "The computer calculates the trajectory of the proton beam and adjusts it in real time to ensure that it hits the tumour precisely."
Protons, being much heavier than photons and electrons, can easily penetrate tissues and release all their energy when they come to a stop — referred to as the Bragg peak. As they move through the tissue, protons lose minimal energy before sharply hitting their target. A proton beam can be moulded to match the shape of a targeted tumour, ensuring a uniform attack on the tumour.
The substantial set-up cost is the foremost reason why India has only two such centres. Another drawback is the large size of the accelerator.
The centre has three treatment rooms, each with a gantry. "The gantry is like a robotic arm," Laskar explains. "It can move around the patient to deliver the proton beam from any angle." The centre, with its dedicated team of radiation oncologists, medical physicists, and radiation therapists, will initially focus on treating patients with head and neck cancers, apart from paediatric cancers. "These are the cancers where proton therapy has shown the most benefit." It will later expand to treat other types of cancers as well. "We want to make proton therapy accessible for all," he says.
From the cyclotron, the proton travels to a beamline, which consists of several magnets on opposite sides of a tunnel. As the proton passes through, the magnets focus it in the desired direction, directing it to the gantry's treatment room. The gantry uses various technologies, including pencil beam scanning, which directs a very narrow beam of radiation into the area where the tumour is located.
"The walls (of the rooms) have to be of a particular density, of a particular thickness, with conduits and pipes running into kilometres through them at a particular angle. Without such high-quality assurance, the machine's alignments will not happen," Laskar says.

The team had to conduct extensive quality assurance tests to ensure that the machine produced the proton beam accurately. This involved analysing the beam statistics and entering the data into the radiation planning system to validate it. Once the data was validated, it was sent to the Atomic Energy Regulatory Board, which gave it the green light to begin treating patients.
THE START
Proton therapy is not new. Over 60 years ago, particle physicist Robert R. Wilson, a founding director of Fermilab in the U.S., had recognised the therapeutic potential of a proton beam for cancer treatment, and shared his insight with fellow nuclear physicist Ernest O. Lawrence, who won the Nobel Prize for his invention of the cyclotron in 1939. In 1954, a patient was treated for the first time with protons at the Berkeley Lab.
"It is always a challenge to bring accelerator physics into medical clinics," says Manjit Dosanjh, former Senior Advisor for Medical Applications at the European Organization for Nuclear Research or CERN and a Visiting Professor at the University of Oxford. "In those days, multidisciplinary collaboration wasn't so common," she says.
Currently, there are 106 proton therapy centres worldwide (bit.ly/106-centres); India has two — ACTREC and the Apollo Proton Cancer Centre in Chennai. The substantial set-up cost is the foremost reason why India has only two such centres. Another drawback is the large size of the accelerator needed to generate high-energy protons. These factors significantly add to the cost of the therapy: a single course of proton beam therapy may typically cost around `1-1.5 crore.
The costs are also high because the planners have to ensure the centre is financially viable. Laskar points out that several proton treatment centres went bankrupt in many parts of the world because of the low footfall volume due to high treatment costs. And the facility itself involves considerable annual maintenance — which costs upwards of `20 crore.

But since the TMH is a grant-in-aid facility under the Department of Atomic Energy, ACTREC is not mandated to make a profit. Its primary mandate is to provide service, followed by education and research, Laskar says. This means that the centre can treat patients at subsidised rates, much lower than elsewhere. "In the U.S., if I have to send a patient for treatment to, for example, MD Anderson Cancer Center, it costs about $100,000 to $250,000 (about `1.5 crore)," he says.
The charges at the privately run Chennai centre are substantially lower than those abroad. At the Mumbai proton therapy centre, Laskar says, 50% of patients will be treated free of cost; for the others, the charges will be much lower than those in other centres. ACTREC is expected to initially treat around 1,000 patients a year and then treat 3,000 patients a year.
CANCER COSTS
According to findings from the Helmholtz Centre for Heavy Ion Research in Germany, patients who have undergone proton beam therapy have a longer life span than those administered X-ray radiations or other forms of treatment. However, despite its approval in countries such as the United States since 1998, India has been unable to reap the benefits of proton therapy due to concerns about the costs involved.
Yet, cancer is a grave health issue in India today. According to official predictions, one in nine people in India is likely to develop cancer in their lifetime (bit.ly/cancer-incidence).
Other techniques are emerging as game changers in particle therapy; carbon ion radiation therapy has a claimed five-year success rate of 95%.
Treatment expenses have also soared over the years. According to a 2014 study by Sunil Rajpal, who was then with the Institute of Economic Growth in New Delhi, nearly half of those seeking treatment fund it mostly through borrowings and charity. Radiotherapy, the traditional way of cancer treatment, is not categorised as an 'essential service' in the country, and is thus exempt from pricing regulations. Cancer also requires continuous medications, draining funds even after a patient has been cured.
Amid this gloom, ACTREC promises a ray of hope. There is more on the anvil, with two more techniques emerging as game changers in particle therapy. The first uses carbon ion radiation therapy, with a claimed five-year success rate of around 95%. Carbon ion is three times more effective than a proton in damaging cancerous DNA. In the other method — called 'flash' — an intense beam of particles is directed on a patient for less than 100 milliseconds. This method stands out because it allows the application of any particle or ion — from photon or proton to electron or carbon. "As it is independent of the choice of the particle and operates swiftly, one can use a small, cheaper machine," Dosanjh says.
ON THE OTHER HAND...
...Not everybody is gung-ho about proton therapy.
It's good to have a vision about proton beam therapy, but its wider impact should be assessed, says Professor Dinesh Makuny, the head of Radiation Oncology at the Yenepoya Medical College in Karnataka.
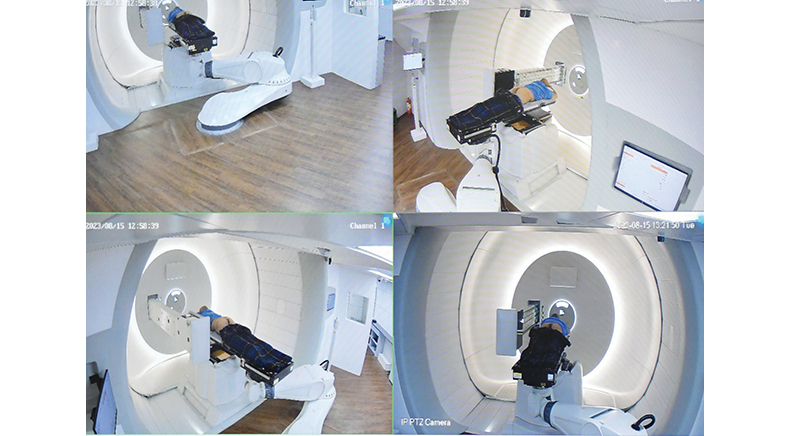
PHOTO: BY SPECIAL ARRANGEMENT
Makuny, earlier a Professor at the Amrita Hospital and the head of Radiation Oncology at the MVR Cancer Centre in Kerala, points out that the Advanced Centre for Treatment, Research and Education in Cancer (ACTREC) will benefit those in need of high-end technology, but will have a more lasting impact if it conducts clinical trials to see the efficacy of proton therapy. A randomised control trial is the highest level of evidence in clinical practice, with no bias involved. But not all high-end machines in proton therapy come through a randomised trial, he says.
For example, he explains, proton therapy for breast cancer to reduce cardiac damage is purely experimental. Such reductions, he adds, are possible even with modern photon therapies. India, he says, needs more linear accelerator machines, commonly used with photons. Maintenance of proton machines is also hugely expensive. "There are no real survival benefits with this technology; in most situations, you may be able to control a bit of cancer for a longer time," he adds.
Have a
story idea?
Tell us.
Do you have a recent research paper or an idea for a science/technology-themed article that you'd like to tell us about?
GET IN TOUCH